|
Introduction
Falls are one of the most common and problematic issues
among older adults (1,2). Generally, one third of community
dwelling older adults had one or more falls each year
(3-6). Falls were the leading cause of injury-related
visits to emergency departments in the United States
(7). Using data from the National Health Interview Survey,
approximately 45% of all injuries in the home environment
leading to medical attention were falls (8). In fact,
20% of nonfatal home falls that require
medical attention occur in the over 75 age group (8).
Moreover, it has been noted
that among individuals who fall, there is a high percentage
(40-73%) who have a fear of falling. It has also been
reported that up to half of older adults who have never
fallen have a fear of falling (3,9). Fear of falling,
whether or not related to a previous fall, can have
a major impact on older adults. Fear of falling may
be a reasonable response to certain situations, leading
elderly persons to be cautious, and can contribute to
fall prevention through careful choices about physical
activity (10). Within this context, fear represents
a reasonable reaction to possible danger and has few
negative consequences as long as physical and social
mobility remains unaffected. However, the fear of falling
can initially present or progress beyond this point
to become a debilitating condition.
In particular, fear of falling
has been associated with negative consequences such
as reduced activity of daily living (11,12), reduced
physical activity (2,13-15), lower perceived physical
health status (16), lower quality of life (2,11), and
increased institutionalization (2,11)
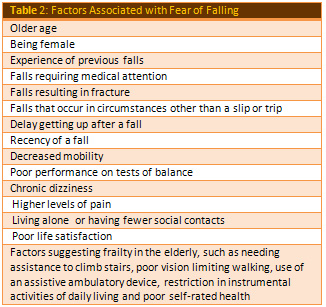
There are many factors associated
with fear of falling, and there are a number of reported
prevention or intervention programs for fear of falling.
However, there is not, as yet, a comprehensive review
of these factors.
Evolution
of the Concept
Despite the importance of the percentage and the consequences
of fear of falling, its definition is still vague and
warrants clarification.
In the late 1970s, Marks and Bebbington described "space
phobia" in four elderly women who had intense fear
of falling "when there was no visible support at
hand or on seeing space cues while driving" (17).
These authors speculated that space phobia "might
be a hitherto unrecognized syndrome or an unusual variant
of agoraphobia". Fear of falling has gained increasing
attention in the public health literature over the past
two decades. The concept was introduced by Bhala, O,
Donnell, and Thopil (18) who used the term "ptophobia
which means a phobic reaction to standing or walking.
Murphy and Isaacs (1982) called it the "post-fall
syndrome" in which elderly people who had fallen
developed severe anxiety that affected their ability
to stand and walk unsupported (19). Subsequent research
demonstrated that elderly people can develop fear of
falling even when they have not fallen (20-22). Other
authors have stated that fear of falling means a patient's
loss of confidence in his or her balance abilities (21,23).
Tinetti and Powell (24) depicted fear of falling as
a progressing worry about falling that at last prompts
evasion of the execution of daily activities. As indicated
by Tidieksaar (25), fear of falling alludes to an un-sound
absence of movement evasion because of dread of falling.
Over the years, various definitions
of fear of falling have evolved. Some authors have focused
purely on the fear (26), while others have included
avoidance of activities as a consequence of the fear
(27). A few authors have eschewed the term "fear"
and have instead focused on the person's loss of confidence
in balance and walking (28,29). Currently the term fear
of falling is used to describe an exaggerated concern
of falling that leads to excess restriction of activities.
The fearful older adult narrows their world, resulting
in isolation and ultimately physical and functional
decline.
So the fear of Falling (FoF)
or Post Fall Syndrome or Psychomotor Regression Syndrome
(PRS) is defined as: "Decompensation of the systems
and mechanisms implicated in postural and walking automatisms
(30)". It appears either insidiously due to an
increase of frailty or either brutally after a trauma
(fall) or an operation. This syndrome is composed of
a combination of neurological signs, motor symptoms
and psychological disorder.
Epidemiology
Among community-dwelling elderly, fear of falling is
frequent, with prevalence ranging from 21 to 61% in
community-based epidemiologic studies (3,20, 26-29,
30). Community studies that are limited to elderly people
who have actually fallen have reported prevalence rates
of 32-83% (31,32). Strikingly, 33-46% of community-dwelling
elders who have not fallen also report fear of falling
(20,21).
Among selected populations, fear of falling has been
found among 46% of nursing home residents, (33) 47%
of persons attending a dizziness clinic,(34) 66% of
patients on a rehabilitation ward,(35) and 30% of hospitalized
elderly patients without a specific diagnosis (40% of
those who had fallen and 23% of those who had not fallen).(11).
Some of these prevalence rates may actually be underestimates,
since people who are most fearful may be less likely
to participate in research studies.
Among elderly persons who are afraid of falling, up
to 70% (20,27,26,30,35) acknowledge avoiding activities
because of this fear. In some cases, individuals become
housebound as a result of their fear. Activity restriction
is, in itself, a risk factor for falls because it can
lead to muscle atrophy, deconditioning and poorer balance
(21, 31). Curtailment of activities can also lead to
social isolation (36). Thus, fear of falling can contribute
to both functional decline and impaired quality of life.
Although a higher prevalence of 40-73% has been reported
in people who have fallen, studies have shown that up
to half of people with fear of falling have not experienced
a fall. These people have likely had a friend or family
member or fellow nursing home resident experience a
fall and have seen the medical and social consequences
for that person.
(3,9,26,36).
Manifestation
Motor symptoms
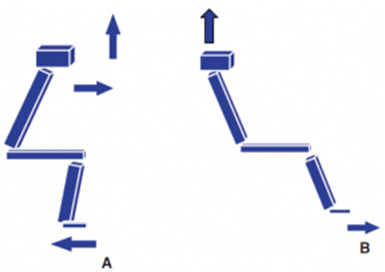
Standing
• "Retropulsion" (gravity center kept
backward)
• Posterior instability (tendency to fall backward)
• Both leading to postural compensation (Knees/hips
kept flexed and bend forward) and to this traditional
posture:

Typical anterior/flexed posture
Sitting
• Impairment of sitting posture is less visible
but as problematic
• Patients with PRS keep their buttocks forward,
shoulders backward and feet far from the seat (image
B)
• However, to stand up we need to transfer our
gravity center forward (image A)
• Therefore, standing up is difficult/impossible
without exterior help for patients with PRS (image B)
A: normal way of
standing up B: wrong way of standing up
Walking
It is difficult for them to
• Initiate the walk (they look like they freeze)
• Difficulty to avoid obstacle and to turn
Gait
•  length of the step
length of the step
•  knees and hips flexion (
knees and hips flexion ( trip risk)
trip risk)
•  heel strike
heel strike
•  time spend in bipodal stance (
time spend in bipodal stance ( posterior instability)
posterior instability)
Neurological signs
o Alteration or absence of postural adaptation (the
person is not able to balance
themselves and to stand up without falling).
o Protective reaction (put their arms in front when
falling to slow the fall)
Psychological disorder
Patient with PRS present with
•
Anxiety/phobia of verticality (afraid to stand
up)
• Loss of self-confidence/self-esteem
• Loss of motivation
associated with a reduction of their activity and social
interaction
Therefore, they end up in a
vicious circle
•
They are afraid to move
• They move
less
• They become
even less able to move and even more afraid
Evaluation
Measurement issues relating to fear of falling
A number of measures have been
developed to measure fear of falling. Each of these
measures uses different definitions and premises. Fear
of falling measures are conceptualized based on the
definition of fear of falling, "fearful anticipation
of a fall" (37), whereas self-efficacy and confidence
measures are based on the individual's confidence or
belief in their ability to perform specific activities
without losing balance or falling.
The FES (28) and Activities-Specific
Balance Confidence Scale (ABC) (38) were developed for
measuring fall related self-efficacy. The FES and ABC
scales have been used repeatedly with community dwelling
older adults (11,13,39-45). Fall-efficacy and confidence
measures, however, may not be a true conceptualization
of fear of falling because it is possible that older
adults feel confident in their abilities to engage in
an activity without "being concerned" about
losing balance or falling, but that they could still
be fearful of having a fall. Additionally, a fear-related
self-efficacy measurement may not be a true conceptualization
as the relationship between the fear of falling and
the self-efficacy to engage in activities is likely
to be strongly influenced by physical function and health
status.
Fear of falling measures
Single item question
The simple question, "Are you afraid of falling?"
was used initially in-research studies with a "yes/no"
or "fear/ no fear" response format (3,40,46).
The advantage of this format is that it is straight
forward and easy to obtain responses. It is limited,
however, as it is not possible to detect variability
in degrees of fear (47), and has an uncertain relationship
to behavior (28). In an attempt to overcome this limitation
some researchers have utilized this single item question
with a Likert scale response pattern (i.e. "not
at all afraid," "slightly afraid," "somewhat
afraid," and "very afraid") to reflect
the degree of fear (45,48,49).
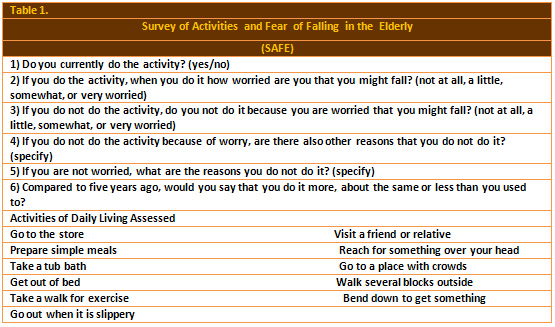
Survey of Activities and fear of falling
in the Elderly
The new instrument Survey of Activities and fear of
falling in the Elderly (SAFFE, Table 1) scale was developed
to assess the role of fear of falling in activity restriction
(50). The SAFFE uses the premise that there are negative
consequences to fear, such as activity restriction or
poor quality of life. The instrument evaluates fear
of falling through the performance of 11 activities
of daily living, instrumental activities of daily living,
mobility tasks, and social activities (i.e., taking
a shower, going to the store, taking public transportation,
and going to movies or shows). Based on the assumption
that activity avoidance may be an early sign of fear
of falling, the SAFFE measures information about participation
in exercise activities and social activities. The SAFFE
has 11 activity items, and for each activity several
questions are asked: (a) Do you currently do it? (yes
or no); (b) If you do the activity, when you do it how
worried are you that you might fall? (0 not at all worried,
1 a little worried, 2 somewhat worried, and 3 very worried);
(c) If you do not do the activity, do you not do it
because you are worried that you might fall? (0 not
at all worried; 3 very worried); (d) If you do not do
the activity because of worry, are there also other
reasons why you do not do it? (if yes, specify); (e)
For those who are not worried, why do you not do it?
(specify); (f) Compared with 5 years ago how often do
you do it? (1 more than you used to, 2 about the same
or 3 less than you used to). However, SAFFE is so complicated
that it is not easy to administer to the elderly. Also,
it is difficult to compute the SAFFE score, because
it is made up of a skip pattern (51). The questions
(a), (b), and (f) determine activity level, fear of
falling status, and activity restrictions, while questions
(c), (d), and (e) examine the number of activities that
are not done because of other reasons in addition to
fear of falling. In addition, the scoring range is 0-33.
SAFFE is not perfect since the instructions on measurement
do not elucidate whether activity and social activity
should be divided when it is computed. Furthermore,
there is no definition of a cut off score that means
fear of fall vs. non fear of fall status. Moreover,
SAFFE measures the degree that elderly feel worry during
periods of activity, while fear of falling while inactive
status is not measured.
The University of Illinois
at Chicago Fear of Falling Measure
Velozo and Peterson (52) developed
the University of Illinois at Chicago Fear of Falling
Measure (UIC FFM) for the community dwelling elderly.
It comprises 16 items and centers on the older adults'
ability to perform activities of daily living. The measure
asks the participants to indicate how worried they would
be if they were to perform the activities. It is a four-point
rating scale. The evidence of reliability of the UIC
FFM was provided by alpha coefficient ( 0.93) (Velozo
& Peterson), but the authors did not report any
evidence of validity.
Fall efficacy measures
Fall efficacy has been used
to measure fear of falling in many studies. However,
as noted before, its conceptualization differs from
fear of falling. Tinetti et al. (28) developed the FES.
The FES is a 10 question scale, and the scores are summed
to give a total score between 0 and 100. Although many
authors have used the FES scale (11,13,40-42,44,45,53),
the measurements are limited because the 10 items measure
only simple indoor activities. The FES, therefore, is
not appropriate for use with older adults who spend
time outside the home and have high mobility (47). An
upgraded version, the modified FES (mFES), contains
an additional four questions about outdoor activities
(29), and has been used in various settings (40).
Activities-Specific Balance Confidence Scale
Powell and Myers (38) developed
the ABC for older adults with greater functioning, based
on the definition of fall related self-efficacy as the
FES. It is a 16-item questionnaire with a visual analog
scale (0-100). The 16-item activities are more specific
than those of the FES. The activities were performed
outside of the home and were more challenging than those
in the FES (16,43).
Fear of falling is one of the
major issues relating to the overall health of older
adults. Fear of falling leads to physical and psychological
problems, and despite the large number of older adults
who suffer from the serious consequences of fear of
falling, its definition is still vague and warrants
clarification. From the literature review, it can be
seen that the most widely used fear of falling measurements
involve the evaluation of fear of falling and fall efficacy.
These measurements need to be used appropriately, based
on the correct definition of fear of falling. Normally,
fear-related efficacy was measured with exact measurements,
such as FES and ABC (54,55). However, when the study
related to the measurement of fear of falling, these
measurements were often misused. Fear of falling was
regularly measured with either fear of falling instruments
(50) or fall efficacy measurements (56-58).
Due to the misinterpretation
and the misapplication of measurements, the percentage
of people suffering from fear of falling may have been
underestimated or overestimated. Therefore, in future
research the question of whether or not the FES accurately
measures fear of falling must be considered. This can
be accomplished by applying both fear of falling measurements
and fall efficacy instruments to the same study participants.
Moreover, nurses working closely with older adults need
to be aware of the different definitions of fear of
falling and the FES. Although older adults may have
a fear of falling, they may also have confidence in
their capabilities to perform activities without falling.
Therefore, nurses may be able to encourage sedentary
older adults who have a fear of falling to perform specific
activities that reinforce confidence with regard to
not falling. Differentiating between the meanings of
fear of falling and fall efficacy is very important
when encouraging older adults to participate in certain
activities. In short, fear of falling needs to be measured
accurately with fear of falling instruments. In addition,
fall efficacy or confidence as it relates to activities
that can be performed without fear of falling should
be measured by using the FES in an effort to clearly
define each variable.
Assessment
Tools
Several approaches to the assessment and measurement
of fear of falling have been used and may partly explain
the variability in the prevalence rates reported above.
The easiest way is to ask subjects the following question:
"Are you afraid of falling?" An annex of this
definite method is to rate the severity of fear, ranging,
for example, from mildly, moderately or very afraid.
Though a direct question is simple, up-front and simply
produces prevalence estimates, this method lacks the
sensitivity of a continuous measure. Tinetti and colleagues
operationalized fear of falling as low perceived self-efficacy.
Self-efficacy refers to an individual's perception of
capabilities within a particular domain of activities
(59). Tinetti, et al. developed the Falls Efficacy Scale
(FES), a 10-question self-rated scale assessing a person's
confidence in performing activities in the home (e.g.,
"How confident are you that you can take a bath
or a shower without falling?"). (28). The subject
rates each question from 1 to 10, resulting in a summative
global score whereby a higher score is reflective of
lower confidence. The scale has been modified for patients
with strokes [FES (S)] (60) and to include outdoor activities
(MFES). (29).
In 1995, Powell and Myers developed the Activities-specific
Balance Confidence Scale (ABC); also based on the self-efficacy
concept (38). This 16-item scale contains a broader
range of activity difficulty and more detailed activity
descriptors than the FES. It has greater reliability
than the FES in detecting loss of confidence in seniors
who are otherwise highly functioning (38).
Lachman, et al. developed the Survey of Activities and
Fear of Falling in the Elderly (SAFFE, table 1), which
examines 11 activities of daily living, instrumental
activities of daily living, mobility tasks and social
activities, using the questions listed in Table 1 for
each activity (50). In contrast to the FES, the SAFE
does not require subjects to make hypothetical responses
about activities that they do not actually perform.
Associated Factors and Comorbidities
Only 10-15% of falls result in fractures or soft tissue
injuries severe enough to cause immobilization or hospitalization
(61). Thus, factors other than physical injury also
play a role in the development of fear and restriction
of activities following single or repeated falls. To
date, studies that have examined correlates of fear
of falling have primarily focused on demographic, physical
and social variables. Multiple variables have been found
to be associated with fear of falling, including those
listed in Table (2) (20,27,28,32,34,35). Thus, like
falling itself, fear of falling is multifactorial in
origin.
A few studies have also employed depression and anxiety
screening scales (4, 7,9,14,16,17). Most, but not all,
of these studies found more severe scores of depression
and/or anxiety among persons with fear of falling compared
with those who are not fearful. In these studies, depression
and anxiety scores were highly correlated. Dowton and
Andrews found that, of eight variables studied, depression
and anxiety scores were the two most important predictors
of chronic dizziness which, in turn, was significantly
associated with fear of falling (20). One study found
that fallers with a fear of falling were significantly
more likely to score above 11 on the Geriatric Depression
Scale (26). This score is frequently used as a cut-off
point to indicate mild or more severe depression, raising
the possibility that minor or major depressive disorders
may be more prevalent among fearful than non- fearful
fallers. However, to date there has been no attempt
to actually determine, by means of diagnostic interviews,
whether depressive and anxiety disorders are more prevalent
in fearful fallers. Furthermore, there has been no attempt
to determine whether specific personality traits or
coping styles predict fear of falling.
Risk factors for fear of falling
Several factors that have been
reported to influence fear of falling including:
Demographic influence
Increased age has been linked to increase in the fear
of falling (3,9,48). However, in studies by Kressig
et al. (41) and Andresen et al. (56), no significant
correlation was found between age and fear of falling.
In addition, women were regularly more likely to be
fearful of falls than men in several studies (3,15).
History of falls
Having had a previous fall was consistently correlated
with a fear of falling (3,15,48,56). Furthermore, multiple
fallers and those who had a harmful fall had a higher
chance of developing a fear of falling than single fallers
(15). However, there are also individuals who have not
fallen who account fear of falling (3,9,48).
Physical health
Fear of falling has been considerably associated with
health status (3,11,15). Those with lower alleged health
status were more liable to have a fear of falling (48).
For instance, Cumming et al (11) completed a prospective
study over 1 year with older adults who had received
medical intervention at the baseline of study. They
found that those who had low fall-related self-efficacy
were more likely to have a poorer health status measured
by health-related quality of life measures and SF-36.
Furthermore, in a study by Fletcher & Hirdes,(15)
poor perceived health status was found to be a risk
factor for activity limitations due to fear of falling
(odds ratio 1.82; 95% confidence intervals 1.47-2.26).
Morbidity
Fear of falling is more prevalent in persons with a
history of neurological problems (i.e., stroke and Parkinson's
disease), cardiac disease, arthritis, osteoporosis,
cataracts/glaucoma, visual and cognitive impairments,
and acute illness (3,11,15,56,61,62). These medical
ailments effect balance and function and hence augment
the individual's fear of falling. Patients with impaired
gait had a greater risk of fear of falling (15,31).
In addition, impaired mobility was associated with a
fear of falling (56,61).
The impact of mood on fear
of falling
Depression and anxiety were emphatically connected with
fear of falling among community dwelling older adults
(41,48,56,63-65). In spite of the fact that a causal
connection amongst depression and fear of falling can't
be deduced from cross-sectional investigations, it is
likely that fear of falling can prompt movement limitation
or social separation, which at that point brings about
discouragement in the elderly (64,66). It has likewise
been speculated that depression and/or the prescription
being take to treat depression adds to falls and a related
fear of falling (64).
The impact of exercise on fear of falling
Fear of falling decreases in older individuals engaged
in exercise programs, including activities to ameliorate
lower limb strength, balance, stability, and continuance,
or Tai Chi exercises (16,42,45,53,67). It is likely
that these activities upgraded lower leg quality, strolling
speed, adjust control, and physical capacity, which
diminished fall rates, and diminished the probability
of a related fear of falling.
Cognitive status
Fear of falling is predominant in older adults, and
may be even more common in populations known to have
balance problems, such as is the situation in individuals
with Parkinson's disease and dementia patients (68).
While cognitive status has not
reliably been related with fear of falling, the reality
of the matter is that some studies point to cognitive
status just like a critical factor in connection to
fear of falling among older adults in the community
(31,68). Specifically, fear of falling was more apparent
in Parkinson's patients with gait impairment than in
healthy older adults (68).
However, fear of falling with
active restriction was not related with older adults'
reported memory problems (12,15). It might be that fear
is extremely founded on cognitive function, but asking
questions relating to fear of falling to persons with
dementia poses a problem since their answers may not
be valid.
Management
Despite the high prevalence of fear of falling and its
associated morbidity, there has been little research
into its management.
Two fall prevention studies included falls efficacy
or fear of falling as a secondary measure. Tinetti,
et al. found that a multiple risk factor intervention
strategy resulted in a significant reduction in risk
of falling and a significant improvement in FES scores
among elderly people living in the community (69). On
the other hand, Reinsch, et al. found that a combination
of exercise, education and relaxation training did not
have a significant effect on the probability of falling
or fear of falling (70).
Three randomized controlled trials have examined the
effect of interventions on falls efficacy and/or fear
of falling as the primary outcome variable. Tennstedt,
et al. evaluated an intervention specifically designed
to reduce fear of falling and improve self-efficacy
in a population of community-dwelling elderly who reported
restriction in activity due to fear of falling (53).
Their cognitive behavioural intervention program had
an immediate, but modest, effect in improving subjects'
self-efficacy and increasing their level of intended
activity. However, these positive effects were not present
at six-month follow-up. Wolf, et al. found a statistically
significant reduction in fear of falling, as well as
risk of falling, among elderly people randomized to
15 weeks of Tai Chi compared to those in the control
condition (45).
Finally, Cameron, et al. found that the use of hip protectors
in elderly women who had fallen in the previous year
had no statistically significant effect on fear of falling,
but was associated with improved self-efficacy (40).
On the basis of these studies, with their varied interventions
and disparate results, it is difficult to derive recommendations
regarding the management of fear of falling. The multifactorial
nature of fear of falling suggests that a multifaceted
approach utilizing both psychological and physical interventions
may stand the best chance of success, but this remains
to be determined in future research. Furthermore, it
is quite possible that the approach to managing fear
of falling in non-fallers will differ from the approach
needed for fallers.
A successful management for patient suffering from Post
fall syndrome is composed of:
o Exercise to stimulate movement and strength
o Postural work to fix the compensation
o Teaching patients the right maneuver on the change
of position to explain the easy
and safe way to stand up, sit down, and lie down.
o Attempt to correct their gait
There are a larger number of
modifiable risk factors (i.e., exercise, physical health,
morbidity, history of falls, and mood status) than non-modifiable
risk factors (i.e., demographic status and cognitive
status) related to fear of falling.
Therefore, the team working
with older adults must work with them to make positive
changes to these modifiable factors by improving and
augmenting their physical activity. Since, depression
is one of the critical issue linked to fear of falling
(71) any strategy to decrease fear of falling should
include depression management. A number of authors carried
a number of intervention studies with the aim of preventing
or managing fear of falling in older adults. It was
clear that exercise programs, including strength training,
balance, endurance, mobility, and Tai-Chi programs,
have confirmed effectiveness in decreasing fear of falling
in older adults (39,42,43,45,53,71,72,73). Furthermore,
a meta- analysis revealed that exercise intervention
is an effective way to diminish fear of falling (58).
In this study, combined exercise programs with education
and cognitive intervention were more effective than
exercise programs alone. Furthermore, exercise within
facility was less effective than home or community-based
exercise (58).
Therefore making information
about fall-related fear to older adults available within
the community will entice fallers to minimize fall-related
accidents and manage fear of falling by taking part
in regular physical activities.
Future
Directions
Fear of falling is one of the major issues relating
to the overall health of older adults. Fear of falling
leads to physical and psychological problems, and despite
the large number of older adults who suffer from the
serious consequences of fear of falling, its definition
is still vague and warrants clarification.
Further research is needed in order to better understand
the genesis of fear of falling, improve its management
and diminish its consequences. It would be of interest
to clarify variables that may predict which individuals
develop fear of falling as an "appropriate"
or "protective" response to falls versus those
in whom the fear is clearly pathological. A greater
research focus on the psychological and psychiatric
correlates of fear of falling would be helpful in this
regard. Furthermore, it will be important to determine
whether interventions that place greater emphasis on
the specific treatment of depression, anxiety, negative
cognitions and avoidant behaviors can result in improved
outcome among older people with fear of falling.
References
1. American Geriatrics Society, British Geriatrics Society,
& American Academy of Orthopedic Surgeons Panel
on Falls Prevention. (2001). Guideline for the prevention
of falls in older persons. Journal of the American Geriatrics
Society, 49, 664-672.
2. Li, F., Fisher, J., Harmer,
P., McAuley, E., & Wilson, N. L. (2003). Fear of
falling in elderly persons: Association with falls,
functional ability, and quality of life. Journal of
Gerontology: Psychological Sciences & Social Sciences,58,
283-290.
3. Friedman SM, Munoz B, West
SK, et al. Falls and fear of falling: Which comes first?
A longitudinal prediction model suggests strategies
for primary secondary prevention. J Am Geriatr Soc 2002;50:1329-35.
4. Means, K. M., Rodell, D.
E., & O'Sullivan, P. S. (2005).
Balance, mobility, and falls among community-dwelling
elderly
persons. American Journal of Physical Medicine &
Rehabilitation, 84,
238-250.
5. Tinetti, M. E. (2003). Preventing
Falls in Elderly Person. The New England Journal of
Medicine, 348, 42-49.
6. Tromp, A. H., Pluijm, S.
M. F., Smit, J. H., Deeg, D. J. H. Bouter, L. M., &
Lips, P. (2001). Fall risk screening test: A prospective
study on predictors for falls in community-dwelling
elderly. Journal of Clinical Epidemiology, 54, 837-844.
7. Fuller, G. F. (2000). Falls
in the elderly. American Family Physician, 61, 2156-2168.
8. Runyan, C. W., Perkis, D.,
Marshall, S. W., Johnson, R. M., Coyne-Beasley, T.,
Waller, A. E., et al. (2005). Unintentional injuries
in the home in the United States: Part II: Morbidity.
American Journal of Preventive Medicine, 281, 80-87.
9. Murphy, S. L., Dubin, J.
A., & Gill, T. M. (2003). The development of fear
of falling among community-living older women: Predisposing
factors and subsequent fall events. The Journal of Gerontology;
Biological Sciences and Medical Sciences, 58, 943-947.
10. Murphy, S. L., William, C. S., & Gill, T. M.
(2002). Characteristics associated with fear of falling
and activity restriction in community-living older persons.
Journal of the American Geriatric Society, 50, 516-520.
11. Cumming RG, Salked G, Thomas
M, et al. Prospective study of the impact of fear of
falling on activities of daily living, SF-36 scores,
and nursing home admission. J Gerontol 2000;5:M299-305.
12. Martin, F. C., Hart, D.,
Spector, T., Doyle, D. V., & Harari, D. (2005).
Fear of falling limiting activity in young-old women
is associated with reduced functional mobility rather
than psychological factors. Age and Ageing, 34,281-287.
13. Bruce, D. G., Devine, A.,
& Prince, R. L. (2002). Recreational physical activity
levels in healthy older women: The importance of fear
of falling. Journal of the American Geriatrics Society,
50, 84-89.
14. Delbaere, K., Crombez, G.,
Vanderstraeten, G., Willems, T., & Cambier, D. (2004).
Fear-related avoidance of activities, falls and physical
frailty. A prospective community-based cohort study.
Age and Ageing, 33, 368-373.
15. Fletcher, P. C. & Hirdes,
J. P. (2004). Restriction in activity associated with
fear of falling among community- based seniors using
home care services. Age and Ageing, 33, 273-279.
16. Brouwer, B., Musselman,
K., & Culham, E. (2004). Physical function and health
status among seniors with and without a fear of falling.
Gerontology, 50, 135-141.
17. Marks I, Bebbington P. Space
phobia: syndrome or agoraphobic variant? BMJ 1976;2:345-7.
18. Bhala, P., O, Donnell, J.,
& Thoppil, E. (). Ptophobia: Phobic fear of falling
and its clinical management. Physical Therapy,1982;
62(2),187-190.
19. Murphy J, Isaacs B. The post-fall syndrome: A study
of 36 elderly patients. Gerontology 1982;28:265-70.
20. Dowton JH, Andrews K. Postural
disturbance and psychological symptoms amongst elderly
people living at home. Int J Geriatr Psychiatry 1990;5:93-8.
21. Maki BE, Holliday PJ, Topper
AK. Fear of falling and postural performance in the
elderly. J Gerontol 1991;46:M123-31.
22. Lawrence RH, Tennstedt SL,
Kasten LE, et al. Intensity and correlates of fear of
falling and hurting oneself in the next year. J Aging
Health 1998;10:267-86.
23. Tinetti, M. E., Speechley,
M., & Ginter, S. F. (1988). Risk factors for falls
among elderly persons living in the community. New England
Journal of Medicine, 319,1701-1707.
24. Tinetti, M. E. & Powell,
L. (1993). Fear of falling and low self-efficacy: A
case of dependence in elderly persons. [Special Issue]
Journal of Gerontology, 48, 35-38.
25. Tideiksaar, R. (2002). Falling
in Older People: Prevention and Management. (3rd ed.),
New York: Springer.
26. Arfken CL, Lach HW, Birge
SJ, et al. The prevalence and correlates of fear of
falling in elderly persons living in the community.
Am J Public Health 1994;84:565-70.
27. Howland J, Lachman ME, Peterson
EW, et al. Covariates of fear of falling and associated
activity curtailment. Gerontologist. 1998;38:549-55.
28. Tinetti ME, Richman D, Powell
L. Falls efficacy as a measure of fear of falling. J
Gerontol 1990;45:P239-43.
29. Hill KD, Schwartz JA, Kalogeropoulos
AJ, et al. Fear of falling revisited. Arch Phys Med
Rehabil 1996;77:1025-9.
30. Tinetti ME, Mendes de Leon
CF, Doucette JT, et al. Fear of falling and fall-related
efficacy in relationship to functioning among community-living
elders. J Gerontol 1994;49:M140-7.
31. Vellas BJ, Wayne SJ, Romero
LJ, et al. Fear of falling and restriction of mobility
in elderly fallers. Age Ageing 1997;26:189-93.
32. Drozdick LW, Edelstein BA.
Correlates of fear of falling in older adults who have
experienced a fall. Journal of Clinical Geropsychology
2001;7:1-13.
33. Franzoni S, Rozzini R, Boffelli
S, et al. Fear of falling in nursing home patients.
Gerontology 1994;40:38-44.
34. Burker EJ, Wong H, Sloane
PD, et al. Predictors of fear of falling in dizzy and
non-dizzy elderly. Psychol Aging 1995;10:104-10.
35. Clague JE, Petrie PJ, Horan
MA. Hypocapnia and its relation to fear of falling.
Arch Phys Med Rehabil 2000;81:1485-8.
36. Howland J, Peterson EW,
Levin WC, et al. Fear of falling among the community-
dwelling elderly. J Aging Health 1993;5:229-43.
37. Silverton, R., & Tideiksaar,
R. (1989). Psychosocial aspects of falls. In R. Tideiksaar
(Ed.), Falling in old age: Its prevention and treatment,
(2nd ed.). New York: Springer.
38. Powell EL, Myers AM. The
Activities-specific Balance Confidence (ABC) Scale.
J Gerontol 1995;50A:M28-34.
39. Brouwer, B., Walker, C.,
Rydahl, S. J., & Culham, E. G. (2003). Reducing
fear of falling in seniors through education and activity
programs: A randomized trial. Journal of American Geriatrics
Society, 51, 829-834.
40. Cameron ID, Stafford B,
Cumming RG, et al. Hip protectors improve falls self-efficacy.
Age Ageing 2000;29:57
41. Kressig, R. W., Wolf, S.
T., Sattin, R. W., O'Grady, M., Greenspan, A., Curns,
A., et al. (2001). Associations of demographic, functional,
and behavioral characteristics with activity-related
fear of falling among older adults transitioning to
frailty. Journal of American Gerontology Society, 49,
1456-1462.
42. Nitz, J. C., & Choy,
N. L. (2004). The efficacy of a specific balance-strategy
training programme for preventing falls among older
people: A pilot randomized controlled trial. Age and
Ageing, 33, 52-58.
43. Sattin, R. W., Easley, K.
A., Wolf, S. L., Chen, Y., & Kutner, M. H. (2005).
Reduction in fear of falling through intense Tai-Chi
exercise training in older, transitionally frail adults.
Journal of American Geriatric Society, 53,1168-1178.
44. Wilson, M-M. G., Miller,
D. K., Andresen, E. M., Malmstrom, T. K., Miller, J.
P., & Wolinsky, F. D. (2005). Fear of falling and
related activity restriction among middle-aged African
Americans. Journal of Gerontology: Biological Sciences
and Medical Sciences, 60A, 355-360.
45. Wolf, S. L., Barnhart, H.
X., Kutner, N. G., McNeely, E., Coogler, C., & Xu,
T. (1996). Reducing frailty and falls in older persons:
An investigation of Tai Chi and computerized balance
training. Journal of American Geriatrics Society, 44,
489-497.
46. Evitt, C. P. & Quigley,
P. A. (2004). Fear of falling in older adults: A guide
to its prevalence, risk factors, and con- sequences.
Rehabilitation Nursing, 29, 207-210.
47. Legters, K. (2002). Fear
of falling. Physical Therapy, 82,264-272.
48. Lach, H. W. (2005). Incidence
and risk factors for developing fear of falling in older
adults. Public Health Nursing, 22, 45-52.
49. Rucker, D., Rowe, B. H.,
Johnson, J. A., Steiner, I. P., Russell, A. S., Hanley,
D. A., et al. (2006). Educational intervention to reduce
falls and fear of falling in patients after fragility
fracture: Results of a controlled pilot study. Preventive
Medicine, 42, 316-319.
50. Lachman, M. E., Howland, J., Tennstedt, S., et al.
(1998). Fear of falling and activity restriction: The
survey of activities and fear of falling in the elderly
(SAFE). Journal of Gerontology: Psychological Science
and Social Science, 53, 43-50.
51. Huang, T. T. (2006). Geriatric
fear of falling measure: Development and psychometric
testing. International Journal of Nursing Studies, 43,
357-365.
52. Velozo, C. A. & Peterson,
E. W. (2001). Developing meaningful fear of falling
measures for community dwelling elderly. American Journal
of Physical Medicine & Rehabilitation, 80, 662-673.
53. Tennstedt S, Howland J,
Lachman M, et al. A randomized controlled trial of a
group intervention to reduce fear of falling and associated
activity restriction in older adults. J Gerontol. 1998;53B:
P384-92.
54. Belgen, B., Beninato, M.,
Sullivan, P. E., & Narielwalla, K. (2006). The association
of balance capacity and falls self-efficacy with history
of falling in community- dwelling people with chronic
stroke. Archives of Physical Medicine and Rehabilitation,
87, 554-561.
55. Schott, N. (2008). German
adaptation of the "activities- specific balance
confidence (ABC) scale" for the assessment of falls-related
self-efficacy. Zeitschrift Fur Gerontologie Und Geriatrie:
Organ Der Deutschen Gesellschaft Fuer Gerontologie Und
Geriatrie, doi:10.1007/s00391-007-0504-9.
56. Andersson, A. G., Kamwendo,
K., & Appelros, P. (2008).
Fear of falling in stroke patients: Relationship with
previous falls and functional characteristics. International
Journal of Rehabilitation Research. Internationale Zeitschrift
Fur Rehabilitations forschung. Revue Internationale
De Recherches De Readaptation, 31, 261-264.
57. Gillespie, S. M., &
Friedman, S. M. (2007). Fear of falling in new long-term
care enrollees. Journal of the American Medical Directors
Association, 8, 307-313.
58. Jung, D. Y., Lee, J. H.,
& Lee, S. M. (in press). A meta-analysis of fear
of falling treatment programs for the elderly. Western
Journal of Nursing Research.
59. Bandura A. Self-efficacy
mechanism in human agency. Am Psychol 1982;2:122-47.
60. Hellstrom K, Lindmark B.
Fear of falling in patients with stroke: A reliability
study. Clin Rehabil 1999;13:509-17.
61. Fessel, K. D. & Nevitt,
M. C. (1997). Correlates of fear of falling and activity
limitation among persons with rheumatoid arthritis.
Arthritis Care Research, 10, 222-228.
62. King MB, Tinetti ME. Falls
in community-dwelling older persons. J Am Geriatr Soc.
1995;43:1146-54.
63. Resnick, B., & Junlapeeya,
P. (2004). Falls in a community of older adults: Findings
and implications for practice. Applied Nursing Research,
17, 81-91.
64. Chou, K. L., Yeung, F. K.
C., & Wong, E. C. H. (2005). Fear of falling and
depressive symptoms in Chinese elderly living in nursing
homes: Fall efficacy and activity level as mediator
or moderator? Aging & Mental Health, 9, 255-261.
65. Gagnon, N., Flint, A., Naglie,
G., & Devins, G. M. (2005). Affective correlates
of fear of falling in elderly persons. American Journal
of Geriatric Psychiatry, 13, 7-14.
66. Niino, N., Tsuzuku, S.,
Ando, F., & Shimokata, H. (2000). Frequencies and
circumstances of falls in the National Institute for
Longevity Sciences, Longitudinal Study of Aging (NILS-LSA).
Journal of Epidemiology, 10, 90-94.
67. Warr, P., Butcher, V., &
Robertson, I. (2004). Activity and psychological well-being
in older people. Aging and Mental Health, 8, 172-183.
68. Schoenfelder, D. P., & Rubenstein, L. M. (2004).
An exercise program to improve fall-related outcomes
in elderly nursing home residents. Applied Nursing Research,
17,21-31.
69. Tinetti ME, Baker DI, McAvay
G, et al. A multifactorial intervention to reduce the
risk of falling among elderly people living in the community.
New Engl J Med. 1994;331:821-7.
70. Reinsch S, MacRae P, Lachenbruch
PA, et al. Attempts to prevent falls and injury: a prospective
community study. Gerontologist. 1992;32:450-6.
71. Van Haastregt, J. C., Zijlstra,
G. A., Van Rossum, E., Van Eijk, J. T., & Kempen,
G. I. (2008). Feelings of anxiety and symptoms of depression
in community-living older persons who avoid activity
for fear of falling. American Journal of Geriatric Psychiatry,
16, 186-193.
72. Li, F., Harmer, P., Fisher,
J., McAuley, E., Chaumeton, N., Eckstrom, E., &
Wilson, N.L. (2005). Tai Chi and fall reduction in older
adults: a randomized control trial. Journal of Gerontology:
Biological Science and Medical Science, 60A(2), 187-
73. Zhang, J-G., Ishikawa-Takata,
K., Yamazaki, H., Morita, T., & Ohta, T. (2006).
The effects of Tai-Chi Chuan on physiological function
and fear of falling in the less robust elderly: An intervention
study for preventing falls. Archives of Gerontology
and Geriatrics, 42,107-116.
|