|
Introduction
There is an increasing elderly population and as a result
an increase in the number of elderly patients with significant
morbidity putting a strain on health services. This
is thought to be due to the decline in global fertility
and family size as well as the decline of mortality
in older populations. A community is regarded as relatively
old when the percentage of the population aged 65 and
above exceeds 10%(1).
In the year 2000 only some of the developed countries
experienced population aging, but it is expected that
by the year 2030 it will be experienced by all developed
countries (2).
Currently depression has a prevalence of 5-10% in the
community, and is now a major health problem in the
elderly population(3). Whether due to differences in
how people view mental health in different generations,
most of the elderly patients who present with mood symptoms
often present to their primary care practitioners as
opposed to mental health professionals(4). It is now
becoming such a prevalent illness that it is expected
to be the largest cause of disability by 2030(5).
Symptoms experienced by patients with depression have
been categorised in the ICD-10, with the key symptoms
being a persistent sadness or low mood throughout most
of the day, anhedonia, and fatigue(6). In order to diagnose
someone with depression, they must also have 2 of the
following symptoms; disturbed sleep, lack of concentration,
low self-esteem, reduced or increased appetite, recurrent
thoughts of death or suicide, agitation or retardation,
and guilt.
Several risk factors have been noted to play a role
in the aetiology of depression. Genetic factors have
a major influence, as described by a paper which showed
an estimated heritability of 37% in twin studies and
family studies indicate a two- to threefold increase
in lifetime risk of developing major depressive disorder
among first-degree relatives(7, 8). However genetic
factors are less likely to play a role in late-onset
depression than in early onset depression. Here social
circumstances may be a larger cause, with issues such
as marital status, adverse life events, unemployment
and impaired social support(9). Consistent with this
perspective, numerous social relationship domains show
an inverse association with depression and depressive
symptoms(10). Studies have shown that whilst being single
puts people at a higher risk of depression in women
than men, being married leads to a higher risk of depression
in men than women(11). Notable factors that are more
prevalent in the elderly population than the younger
population are chronic pain and medical illness. This
is because older adults will be more likely to have
substantial co-morbidities and may find these illnesses
more psychologically distressing as they can lead to
increased disability, decreased independence and a disruption
of social networks. This is particularly the case for
patients who have cerebrovascular disease, Parkinson's
disease, epilepsy, and cancer.
Later life depression is a major health problem because
it is associated with an increased risk of morbidity
as shown above, increased risk of suicide, increased
impairment be it physical cognitive or social, and greater
self-neglect. Because of these, there is an increased
mortality associated with depression in the elderly.
Data shows there are two peaks for ages at high risk
of suicide, which are 25-30 year olds and the elderly
population(12).
When looking in more depth at prevalence rates of depression
in the elderly, it has been found that whilst major
depression was rarer (1.8%), minor depression is more
common (9.8%)(13). However it has also been found that
the levels of detection and treatment of depression
are low in the elderly, which is partly due to patient's
refusal to speak freely about their depressive symptoms
as a result of stigmatised beliefs, the fact that somatic
symptoms are less useful to diagnose depression in the
elderly than in the young, and partly to a lack of access
to specialised mental health resources(14). There are
several tools to screen for depression in the elderly
population such as the Hamilton Rating Scale for Depression,
the Geriatric Depression Scale and the Zung Self-Rating
Depression Scale, however the most reliable and valid
measure of geriatric depression is the GDS, with a specificity
of 94%(15). There are two versions of the GDS, one which
is 30 questions long and the other with 15 questions
which was used in this study. Scores ranged from 0 to
15, with scores of 0-4 showing normal result, 5-9 indicating
mild depression, and 10-15 indicating moderate to severe
depression.
Aims
1) To determine the prevalence of depression among elderly
people in Kurdistan.
2) To study the correlates of depression in late life:
Gender, Age, Education level, Economical status, Marital
status, Housing, Alcohol use, Functional status and
History of chronic medical illnesses
Patients & Methods
This is a cross-sectional study of non-institutionalized
participants, aged 65 or more years old, which is based
on multistage random sampling in three main governorates
of Kurdistan, Sulaimani, Hawler and Duhok.
Data was collected from January 2014 to June 2014 in
face to face household surveys of 650 residents of urban
and rural areas.
The structured interview included assessment of socio-demographic
characteristics, mental and physical health, functional
status, drug history, and living arrangements.
Inclusion criteria:
1. Aged 65 years and above.
2. Those who speak Kurdish.
Exclusion criteria were:
1. Patients who had other psychological problems.
2. Those who had dementia.
3. Those who speak Arabic. (those who do not speak Kurdish)
The study was approved by the scientific and the ethical
committee of the University of Sulaimani.The interviews
were conducted by the researchers directly.
Verbal consent was taken from the participant.
Assessment of depression was done using GDS-15.
Scoring of the GDS-15 ranges from 0-15. Indicating the
grade of the depression from no depression to mild,
moderate and severe depression.
We translated the GDS-15 into Kurdish, then retranslated
it to English, then compared them to ensure fewer grammar
errors.
Statistical analysis
Data concerning different variables were entered into
an Excel office spreadsheet. Data analysis was done
by using SPSS (version 20 software) computer program.
The mean values, SD of the measurements were calculated.
To test the relationship between different variables,
comparisons were made using Chi-square testing. All
P- values were based on 2-sided tests, and p < 0.05
was considered statistically significant.
Results
The mean + SD age of study
population was 71.5 + 6.8 years. About 73.3% of them
were below 75 years and 25.7% 75 years old and above.
The majority of the study population were male (61.2%)
and mostly people were married(68.9%). More than half
of the study population were living in Sulaimani (53.5%),
with the remainder living in Hawler and Duhok. Eighty
seven percent of the study population were living in
an urban area. In this study, most of the participants
had 5 children and more (64.5%).
The majority of the study population
lived in their own homes in the community (96.6%), with
only 10.1% of participants living by themselves. Only
27.8% of the study population were in employment, with
moderate economic status dominating (51.5%).
56.0% in this study were ex-smokers
with 21.2% had never smoked. Most study participants
(83.3%) were mobilised without any aids, 14.1% walked
with a stick, and only 2.6% used other aids. About 6.1%
of them had a history of drinking alcohol and 75.5%
used medications for chronic diseases. Across the whole
study 67.2% used 1-2 medications and 32.4% used 3 medications
and above. The percentages of a positive history of
diabetes, hypertension, stroke, ischemic heart disease,
chronic obstructive pulmonary disease, Parkinson's disease,
and other diseases were 26.2%, 46.6%, 6.5%, 10.8%, 11.2%,
7.4%, 30.5% respectively. The mean duration of disease
in the study population was 2.3 + 0.7 years. The mean
times of attacks of disease were 1.7 + 1.3. Despite
multiple co-morbidities about 72% of the population
had no history of hospital admission.
The results show that
most of the study population had mild depression (41.4%),
Table 1.
Table 1: Depression scale according to the severity
of depression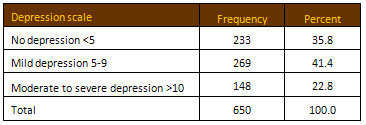
Although most of the study
population who were selected from both the community
and nursing homes had depression (scored 5 - 15), the
relationship between place of abode and depression was
still statistically not significant (P> 0.05). The
relationship between area of residence and depression
scale was also studied and the association was statistically
significant (P=0.031). Most of the study population
in Sulaimani, Duhok, and Hawler had depression (scored
5 - 15), but the highest percentage was in Duhok 73.9%.
The relationship between gender
and depression scale was statistically highly significant
(P<0.01). Females had a higher percentage of depression
(77.4%) than males (55.8%).
The association between gender and depression scale,
according to the severity of depression, was also studied.
The relationship was found statistically highly significant
(P<0.01), i.e. females also had higher percentages
of both (mild) and (moderate to severe) depression (44.4%
and 32.9%) than males (39.4% and 16.3%) respectively,
Table 2.
Table 2: Gender and
grade of depression
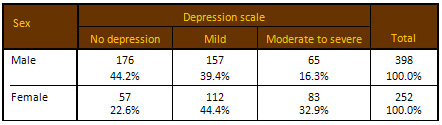
Chi= 39.70, df= 2, P value=
0.000
Our study shows that depression
was more prevalent in those who live in a rented house
or other accommodation (81.1% and 78.7% respectively)
in comparison with those who owned their home (60.5%).
The relationship between type of housing and depression
scale was statistically highly significant (P<0.012).
The association between the history of alcohol use and
depression was studied. It was statistically significant,
P<0.05. Depression was lower in those with a history
of alcohol use (48.7%) in comparison with no alcohol
use (65.3%), P=0.036.
The relationship between the
history of hospital admissions in the last 12 months
and depression scale was statistically highly significant,
P=0.001. Additionally, the highest percentage of depression
was in those with a history of hospital admission (77.1%),
Lastly, a statistically highly significant association
was found between the number of medications used by
the individual and the depression scale, P<0.01.
The highest percentage of depression was found in those
who used 3 medications and above (80.0%).
Table 3 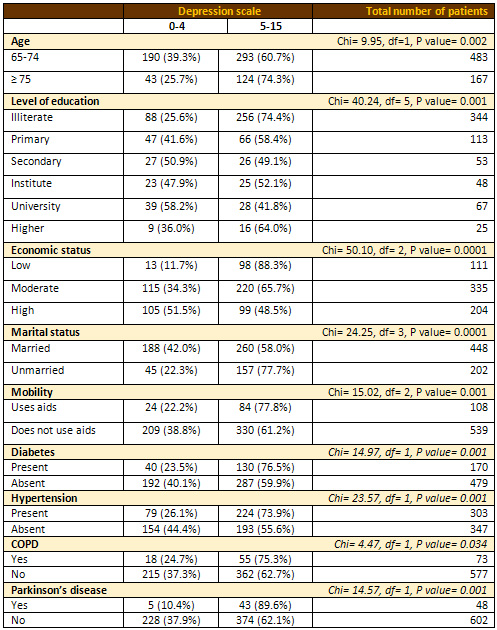
Discussion
This cross sectional study demonstrates that there is
a high prevalence of depression in the elderly, with
64.2% of participants affected, the majority of whom
were suffering mild depression (41.4%) and just under
a third (22.8%) moderately to severely depressed. Given
the majority of the study population were male (61.2%)
and the rate of depression in women was found to be
significantly higher (77.4% vs 55.8%, P-value 0.001),
this may even be a disproportionately low figure. Whilst
this supports the hypothesis the notion that depression
is a mounting issue, it is even more than would be expected.
Furthermore, none of those identified as depressed had
a pre-existing diagnosis of depression. Such high percentage
might be the possibility of Geriatrics Depression scale
questioning only has specificity and sensitivity in
diagnosing depression if asked in English to an English
speaking subjects with western social values and standard
of education in society. However the questionnaire in
this study was transplanted to Kurdish and the subjects
were all Kurdish with middle-eastern social values and
standard of education. Whether the subjects understood
the reasoning for Geriatric Depression Scale questions
when asked would have made a difference.
According to a systematic review of community-based
studies on depression in later life from The Netherlands,
higher percentages of depression were demonstrated in
women(16). The overall prevalence rates were also markedly
lower than found in this study, with the average at
13.5% and a range of 0.4-35%.9 Given the review noted
correlation of low socio-economic situation with depression
and the discrepancy of prevalence between these studies,
it is reasonable to hypothesize that there may have
been higher incidence of such risk factors in this study
population(16).
A review from Brazil, a more comparable developing country,
showed that depression was more prevalent in the younger
elderly (aged 65-74) with no pronounced difference between
the sexes(17). As our study's participants were mostly
under 75, with a mean age of 71.5, this might be one
explanation for its finding such high levels of depression.
Compared to the study in Brazil, the prevalence of depression
in Kurdistan was actually higher in late elderly age
group (75 years and over) (74.3%) compared to early
elderly age group (60.7%), P-value=0.002. Additionally,
a similar study in The Netherlands revealed that the
late elderly age group is at higher risk for developing
depression(18).
That being said, the proportion of participants with
mild vs moderate and severe depression is supported
by an Iranian study of elderly people in a nursing home
in Tehran that revealed higher rates of mild depression
(50%) compared to moderate and severe depression (29.5%
and 10.7% respectively)(19). This data has been mirrored
in other cases, where a study in Canada also revealed
more prevalent rates of mild depression compared to
major depression (2.6% and 4% respectively)(20).
A study in Lebanon showed that elderly people with dementia
were more likely to be depressed, with a prevalence
of 41.2% compared to 14.5% in those without cognitive
impairment(21). Though this study did not specifically
comment on dementia, and given the low proportion that
were from a nursing home it might be assumed to be low,
it would be interesting to have this data. Nevertheless
this supports the evidence that disease is a risk factor
for depression, as shown in our study with higher rates
of depression in those with COPD, Parkinson's, hypertension,
diabetes, hospital admission within a year, reduced
mobility and polypharmacy (with statistical significance
shown for all but COPD).
An interesting point was that smoking did not correlate
with mood, and those who drank alcohol had less risk
of developing depression in our study (P-value 0.036).
There is no data in this study and limited data in general
on whether there is any correlation between religion
and depression, but it may be a factor and even implicated
in the link with alcohol, particularly in this study
given the population is predominantly Muslim.
Residential and nursing home residents generally have
poorer health than those in their own homes and so by
this reasoning would be more at risk of depression.
Supporting this, a study from Turkey exposed that depression
among the elderly population living in nursing homes
was indeed more prevalent than for those living at their
own home, 41% and 29% respectively(22). However living
in nursing home in this study did not increase the chance
of depression (P-value 0.654), though this may be due
to smaller number of nursing home participants.
The prevalence of depression among elderly Pakistanis
in a similar cross-sectional study found higher rates
of depression among those with multiple diseases, financial
problems and taking numerous medications(23). A study
in Brazil has concurred with this point, showing depression
is significantly more common in the presence of medical
diseases, poor functional capacity, and hospital admissions
in the last 12 months.10 Furthermore, in a big Saudi
study involving 7,970 people, depressive symptoms were
found in about 40% and was also shown to be strongly
associated with poor functional capacity and multiple
medical diseases with polypharmacy(24). Additionally
higher prevalence of depression was seen in those with
poor housing conditions, poor educational status, living
in remote areas, the unemployed, divorced or widowed
and women(24). This study highlighted that the single,
widowed, divorced, those with poor economic status,
the illiterate and interestingly also the highly educated,
are more likely to develop depression. Further to this,
those who rented houses rather than owned them were
found to have a higher prevalence.
Conclusion
This study highlights the fact
that depression is a common condition in the elderly
population of Kurdistan. Life expectancy in Kurdistan
is already increasing and it will continue to do so
as part of world-wide increase in the elderly population.
Among the health problems of this age, affective disorders
are becoming apparently common. In order to cope with
these changes, improvement in or even establishment
of health care services to this age group is an essential
health strategy focus that needs to be on both under
and post graduate training in care of the elderly mental
health and public awareness about depression in the
elderly. Health systems must be designed to meet the
needs of the population served.
References
1. Gavrilov L.A., Heuveline
P., Aging of Population, The Encyclopedia of Population.
New York, Macmillan Reference USA, 2003
2. United Nations, Department of Economic and Social
Affairs, Population Division (2015), World Population
Ageing, 2015
3. Pinquart M, Duberstein PR, Lyness JM. Effects of
psychotherapy and other behavioral interventions on
clinically depressed older adults: A meta-analysis.
Aging and Mental Health. 2007;11:645-657.
4. Unützer J, Katon W, Sullivan M, Miranda J. Treating
Depressed Older Adults in Primary Care: Narrowing the
Gap between Efficacy and Effectiveness. The Milbank
Quarterly. 1999;77(2):225-256.
5. Mathers C, Loncar D. Projections of Global Mortality
and Burden of Disease from 2002 to 2030. PLoS Medicine.
2006;3(11):e442.
6. The ICD-10 Classification of Mental and Behavioural
Disorders: Diagnostic criteria for research [Internet].
10th ed. Geneva: world health organisation; 2017 [cited
1 February 2017]. Available from: http://www.who.int/classifications/icd/en/GRNBOOK.pdf
7. Sullivan P, Neale M, Kendler K. Genetic Epidemiology
of Major Depression: Review and Meta-Analysis. American
Journal of Psychiatry. 2000;157(10):1552-1562.
8. Lohoff F. Overview of the Genetics of Major Depressive
Disorder. Current Psychiatry Reports. 2010;12(6):539-546.
9. Barger S, Messerli-Bürgy N, Barth J. Social
relationship correlates of major depressive disorder
and depressive symptoms in Switzerland: nationally representative
cross sectional study. BMC Public Health. 2014;14(1).
10. Cacioppo J, Hawkley L, Ernst J, Burleson M, Berntson
G, Nouriani B et al. Loneliness within a nomological
net: An evolutionary perspective. Journal of Research
in Personality. 2006;40(6):1054-1085.
11. Umberson D, Montez JK. Social Relationships and
Health: A Flashpoint for Health Policy. Journal of health
and social behavior. 2010;51(Suppl):S54-S66.
12. Conwell Y, Van Orden K, Caine ED. Suicide in Older
Adults. The Psychiatric clinics of North America. 2011;34(2):451-468.
doi:10.1016/j.psc.2011.02.002.
13. Beekman A T, Copeland J R, Prince M J, Review of
community prevalence of depression in later life, The
British Journal of Psychiatry Apr 1999, 174 (4) 307-311;
DOI: 10.1192/bjp.174.4.307
14. Lyness J, Cox C, Curry J, Conwell Y, King D, Caine
E. Older Age and the Underreporting of Depressive Symptoms.
Journal of the American Geriatrics Society. 1995;43(3):216-221.
15. Yesavage J, Brink T, Rose T, Lum O, Huang V, Adey
M et al. Development and validation of a geriatric depression
screening scale: A preliminary report. Journal of Psychiatric
Research. 1982;17(1):37-49.
16. Beekman AT, Copeland JR, Prince MJ. Review of community
prevalence of depression in later life. The British
Journal of Psychiatry 1999; 174:307-311.
17. Luis BS, Baxter S, Gerada GF, Fabio G. Depression
morbidity in later life: Prevalence and correlates in
a developing country. The American Journal of Geriatric
Psychiatry 2007;15 (9): 790-799.
18. Licht-Strunk E, van der Kooij KG, van Schaik DJ
F, van Marwijk HWJ, van Hout HPJ, de Haan M. and Beekman
ATF. Prevalence of depression in older patients consulting
their general practitioner in The Netherlands. Int.
J. Geriat. Psychiatry 2005; 20: 1013-1019.
19. Nazemi L, Skoog I, Karlsson I, Hosseni S, Hosseni
M, Hosseinzadeh MJ, Mohammadi MR, Pouransari Z, Chamari
M, Baikpour M. Depression, prevalence and some risk
factors in elderly Nursing Homes in Tehran, Iran. Iran
Journal of Public Health 2013; 42(6): 559-569.
20. Østbye T, Kristjansson B, Hill G, Newman
SC, Brouwer RN, McDowell I. Prevalence and predictors
of depression in elderly Canadians: The Canadian study
of Health and Aging. Chronic diseases in Canada 2005;
26(4): 93-99.
21. El Asmar K, Chaaya M, Phung KTT, Atweh S, Ghosn
H, Khoury RM, Prince M, Waldemar G, Anxiety among older
adults in Lebanon: preliminary data from Beirut and
Mount. Alzheimer's & Dementia: The Journal of the
Alzheimer's Association, 2014; 10(4): 595-P595
22. Tsuang MT, Faraone SV. The genetics of mood disorders.
Baltimore MD: Johns Hopkins University Press; 1990.
23. Ganatra HA, Zafar SN, Qidwai W, Rozi S. Prevalence
and predictors of depression among an elderly population
of Pakistan. Ageing and Mental Health 2008; 12(3): 349-356.
24. Al-shammari SA, Al-Subaie A. Prevalence and correlates
of depression among Saudi elderly. International Journal
of Geriatric Psychiatry 1999; 14(9): 739-747.
|