|
Introduction
The portion of frail people in the community is increasing.
Since the definition of this syndrome is in development,
the clear numbers of frailty are not well known. A systematic
review estimated the prevalence of frailty in the community
ranging between 4-59.1% (1), which depended on the definition
of frailty. Based on the Fried model it was found as
9.9% and 44.2% for frailty and pre-frailty respectively
(2,3).
In Turkey recent studies have reported different frequencies.
Akin S et al (4) reported in community-dwelling Turkish
elderly a prevalence of frailty, pre-frailty and non-frailty
measured with the modified Fried Frailty Index as 27.8,
34.8, and 37.4 %, respectively and 10, 45.6, and 44.4
% with FRAIL scale. Eyigör et al. (5) found 39.2
and 43.3 % of patients attending outpatient clinics
of 13 university and training hospitals as frail and
pre-frail, respectively. Çakmur H (6) reported
in a rural city sample from East Turkey 7.1% frail and
47.3% pre-frail according to Fried Frailty criteria.
Frailty is a difficult process, which affects the patient
and the garegivers. Conditions, which develop with aging
and disablity are a burden to the person and their family.
Preventive measures have been recommended in the past
to overcome this problem (3). Proper and early intervention
might ameloriate the outcomes of this problem, which
is proven by evidence (3).
The identification of frailty is important and family
practice plays a central role. The family physician
can deliver an holistic approach to manage frailty.
Low-resourced settings and places with accessibility
problems might especially benefit from this (7,8), but
established well-developed health care systems also
could profit from a person-centred approach.
The detection of frailty could follow an opportunistic
pathway, where formal and informal health care and social
service professionals could be useful. Further services
of professionals, who are not especially trained for
this risk group (midwifes, mother and child care nurses)
could be utilised for this purpose (3). The information
reftrieved from the caregiver might be an important
source for early identification of these patients, who
are in need of help and support. A patient-centred approach
focusing on self-preceived care needs is a relatively
unknown approach of needs assessment in frail elderly.
It is as important as the geriatric assessment (9,10).
So far, we are not aware of any study, which is evaluating
the contribution of caregivers for the identification
of the frail person at home.
This study aims, to investigate by asking attendants
to a family practice, the SARC-F scores of frail people
at home and the opinion of caregivers on the care of
the frail.
Materials
and Methods
Research design: This cross-sectional study included
1,016 patients, who consecutively visited a family practice
outpatient clinic in Antalya, Turkey and who voluntarily
participated in this study. The study took place between
March-October 2015. The
participants had educational level of at least primary
school level.
The questionnaire had two steps. Firstly all participants
were asked if they had a frail person at home for whom
they were in charge of. The definition of frailty was
made according to the definition stated in the document
(Frailty is a multidimensional geriatric syndrome characterized
by increased vulnerability to stressors as a result
of reduced capacity of different physiological systems.
It has been associated with an increased risk of adverse
health-related outcomes in older persons, including
falls, disability, hospitalizations and mortality, and
has further been associated with biological abnormalities
(e.g. biomarkers of inflammation) regardless of the
definition used to assess frailty. This clearly suggests
that frailty is influenced by a number of pathophysiological
modifications involving the body's diverse physiological
systems. http://www.frailty.net/frailty-at-a-glance)
(11). The participants gave verbal consent.
Instrument development:
The questionnaire was developed as follows: Firstly,
the literature (1,2,12,13) and short frailty questionnaires
(i.e. SARC-F) were evaluated (14). The draft questionnaire
was evaluated by independent experts from family practice
with a special interest in elderly care and frailty
and afterwards pilot-tested with a total of ten patients.
The pilot survey was excluded from the final database.
This process enabled refined and improved items with
clarity in the wording of the survey.
The survey had the following
sections:
a. Demographics: 2 open-ended (i.e. age
of the participant and frail elder) and 7 closed-ended
questions (i.e. gender, marital status, frail elder
at home; age, drugs, polypharmacy, and disease of the
frail elder);
b. SARC-F items (15,16,17): Strength,
assistance walking, rise from a chair, climb stairs,
and falls are included in the SARC-F items. Scores range
from 0-10. Each item counts for 0-2 points. Total score
ranges are between 0 = best to 10 = worst. Outcome of
total score was dichotomized to symptomatic (frail)
(4+) and healthy (0-3) status. In this study the caregiver
was asked "how much difficulty (the older person
at home) had lifting or carrying 5 kg" (0 = no
difficulty, 1=some, and 2 = a lot or unable to do);
"how much difficulty (the older person at home)
had walking across a room" (0 = no difficulty,
1=some difficulty, and 2 = a lot of difficulty, use
aids, or unable to do without personal help); "how
much difficulty (the older person at home) had transferring
from a chair or bed" (whether they used aids or
needed help to do this) (0 = no difficulty, 1=some difficulty,
and 2 = a lot of difficulty, use aids, or unable to
do without help); "how much difficulty they had
climbing a flight of 10 steps" (0 = no difficulty,
1=some, and 2 = a lot or unable to do),and falls was
scored a 2 for respondents who reported falling four
or more times in the past year, 1 for respondents who
reported falling 1-3 times in the past year, and 0 for
those reporting no falls in the past year.
c. Attitudes and Perception
on the Care of their Frail Elder:
Participants were asked to rate the following questions
on a five-point Likert scale (strongly disagree to strongly
agree, scored from "1" to "5"):
"I feel competent in caring for my frail elder",
"I would follow the treatment recommendations of
my frail patient", "I would seek appropriate
support for my frail elder", "Immobile, frail
elder need home health services", "The family
plays an important role in the early diagnosis of frailty",
"Mobile technologies play an important role in
the care of frail elders", and "Family members
play an important role in the care of frail elders".
Statistical analysis:
Data of this study were analysed with descriptive statistics;
chi-square for categorical variables and Spearman's
rho correlation. The level of significance was set at
alpha=0.05.
Results
The age of caregivers of frail people were 52.1 (SD=12.66;
min-max=19-83; n=1016). Most were women (N=762; 74.9%;
men n=256;25.1%) and married (n=722; 75.1%; divorced/widowed,
n=165;17.2%; single, n=74; %7.7; missing value, n=57,
5.6%)). One hundred and sixty nine (16.8%; n=14 missing
values, %1.4) patients indicated to have a frail person
at home.
The age was 78.2 (SD=8.21; min-max=55-98;
n=170). Most were women (n=124; 75.6%; male, N=40; 24.4%;
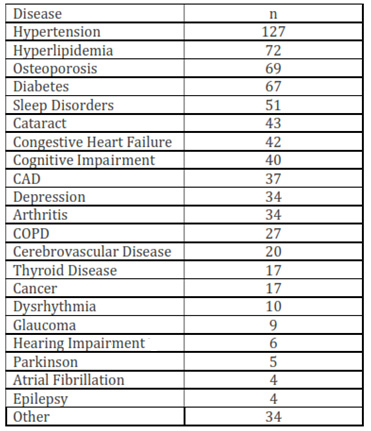
n=854, %83.9 missing values). Disease of the frail elderly
is shown in Table 1 (median= 1 disease; min-max=0-4).
Table 1: Diseases of the frail person
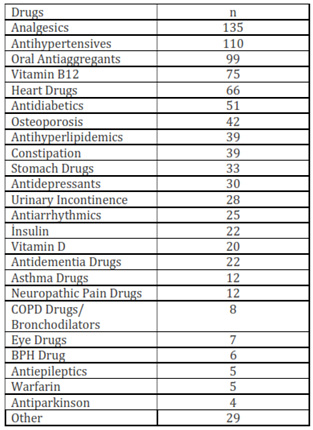
Most frail persons (84%) used
more than four drugs a day. The drugs used by the frail
patient are shown in Table 2 (median 6 drugs; min-max=0-14).
One hundred and twenty nine (75%) patients used four
and more drugs.
Table 2: Drugs used by the frail patient
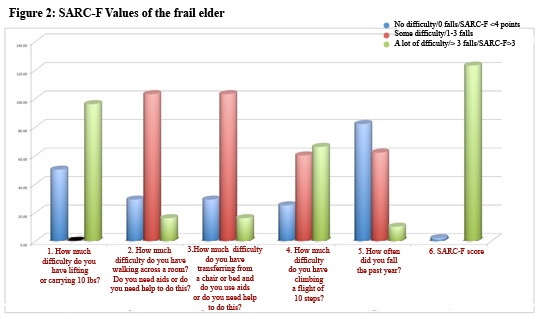
Sarc-F Total Score was found
to be 5.2 (median=5; SD=1.1; min-max=3-8; n=125) (Figure
1). The frequency distribution of the SARC-F values
of frail people are shown in Figure 2 (SARC-F Score
>=4=99.8%; 4-6=85.2%). SARC-F>=4 was prevalent
in 123 elderly, which was 12.1% of all participants
in this study.
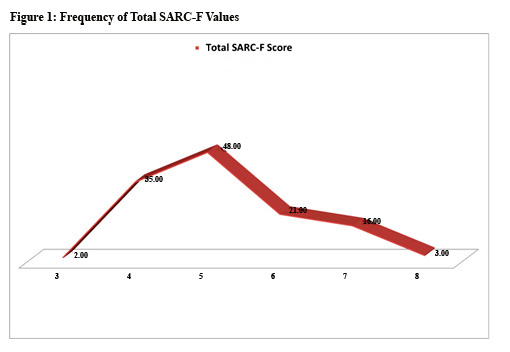
Figure 2: SARC-F Values
of the frail elder
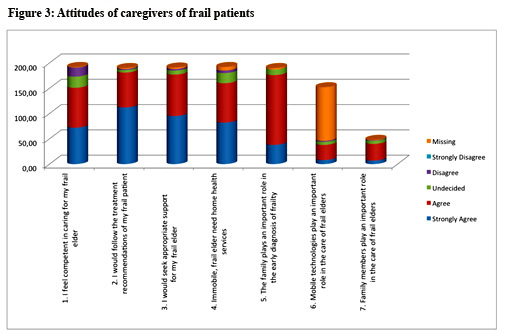
The attitudes of caregivers
of frail people are shown in Figure 3.
The gender of the participants
showed no difference between their age, their frail
elders' age and SARC-F total score (p>0.05). The
gender and the number of medicaments used did not have
an effect on the SARC-F total score (p>0.05).
Total SARC-F score correlated at medium level with the
falls item (r=0.70,p<0.05), walking item (r=0.46,p<0.05),
transfer item (r=0.44,p<0.05), and stairs item (r=0.66,p<0.05).
Attitude of competency to provide care item, correlated
at medium level with following treatment recommendation
item (r=0.49,p<0.05), at low level with seeking appropriate
care item (r=0.33,p<0.05), and at low level with
family members play important role item (r=0.17,p<0.05);
following treatment recommendation item showed medium
level correlation with seeking appropriate care item
(r=0.51,p<0.05), and low level with the role of mobile
technology item (r=0.21,p<0.05); the seeking appropriate
care item showed low level correlation with the early
diagnosis item (r=0.19,p<0.05) and with the role
of mobile technology item (r=0.22,p<0.05); the home
health care item showed low level correlation with role
of mobile technology item (r=0.25, p<0.05); the early
diagnosis item showed low level correlation with role
of mobile technology item (r=0.23, p<0.05) and the
important contribution of the family item (r=0.32, p<0.05).
The falls item of SARC-F showed low-medium level correlation
with the competency to provide care item (r=0.34,p<0.05);
the power item of SARC-F showed low level correlation
with the competency to provide care item (r=0.18,p<0.05);
total SARC-F score correlated at low-medium level with
the competency to provide care item (r=0.31,p<0.05)
and low level with the following treatment recommendation
item (r=0.18,p<0.05).
Discussion
This study showed that the majority of frail people
at home were suffering from at least one (0-4) chronic
condition and 75% used more than four drugs (polypharmacy).
According to SARC-F evaluation most were at pre-frail
level. The domains on upper extremity strength and climbing
stairs were the weakest, which could be improved with
exercise. Short distance walking, transfers and falls
were better. Participants were in agreement with the
statement "I feel competent in caring for my frail
elder", "I would follow the treatment recommendations
of my frail patient", "I would seek appropriate
supprt for my frail elder", "Immobile, frail
elder need home health services", "The family
plays an important role in the early diagnosis of frailty",
"Mobile technologies play an important role in
the care of frail elders", and "Family members
play an important role in the care of frail elders".
Participation in the last two items was low.
The multi-morbidity of our patients in the study was
not high. Cesari et al. report that multimorbidity might
show a moderating effect on related health-care utilisation,
than patients who are not diagnosed with multimorbid
conditions (1). In this case, patients without multi-morbidity
might be at risk of being undetected for frailty condition.
But even if the patient is having a disability or comorbid
condition the diagnosis of frailty does not take this
into consideration. The more the number of chronic conditions
the higher the risk of frailty has been observed (18).
Heart failure, COPD, chronic kidney disease, urinary
incontinence, and cognitive impairement might present
higher prevalence of frailty (19).
But the relation of frailty to aging and chronic conditions
is not clear (18).
According to SARC-F evaluation most were at pre-frail
level. SARC-F has been shown to be a good predictor
of poor muscle function, which has a good correlation
with knee strength and grip strength. It also shows
good correlation with FRAIL scale, which is a self-administred
tool (17). In our study, the domains on upper extremity
strength and climbing stairs were the weakest, which
could be improved with exercise. Short distance walking,
transfers and falls were better.
Our study showed a predominance of women with frailty,
but this observation did not reveal any significant
difference concerning SARC-F score, therefore indication
that the level of frailty was equal in both genders.
A higher prevalance of frailty in women has been also
observed in the literature (1,19).
Most frail people at home were at pre-frail level (SARC-F
Score 4-6=85.2%). In a study, which performed home care
assessments 21.3% were found prefrail and 26.9% frail
(20).
Caregivers were confident, compliant and empowered concerning
the care for their patients. They are aware of home
health care services and would also apply for these.
Another study reported that caregivers, who cared for
the frail were more prone to leave, but caring for pre-frail
patients did not provoke this feeling (20), which is
supported in our findings.
The determination of care needs of frail people is recommended
due to its potential to improve the care of this risk
group. The evaluation of self-perceived health needs
might be a good starting point (21). The results of
our study also provided valuable information on the
situation of patients, who cared for their frail elders
at home. These findings have in our opinion two important
implications. There is a potential need for interventions
to prevent frailty in elderly people at home and a need
to follow-up the health and burden of caregivers. Both
approaches certainly exceed the capacity of family practice.
These need to be managed by a multi-disciplinary healthcare
and rehabilitation team, where the family physician
should be a member. The family physician and his team
could contribute to the management of this problem by
screening caregivers, healthy (13,22), and possible
frail elders, performing home visits, training caregivers
concerning warning signs of frailty, and empowering
elderly people concerning their own health (1,23).
Acknowledgment:
This study has been supported by the Akdeniz University
Research Management Unit.
References
1. Collard RM, Boter H, Schoevers RA, Oude Voshaar RC.
Prevalence of frailty in community-dwelling older persons:
A systematic review. J Am Geriatr Soc 2012;60:1487e1492.
2. Fried LP, Tangen CM, Walston J, et al. Frailty in older
adults: Evidence for a phenotype. J Gerontol A Biol Sci
Med Sci 2001;56:M146eM156.
3. Cesari M, Prince M, Thiyagarajan JA, De Carvalho IA,
Bernabei R, Chan P, Gutierrez-Robledo LM, Michel JP, Morley
JE, Ong P, Rodriguez Manas L, Sinclair A, Won CW, Beard
J, Vellas B.Frailty: An Emerging Public Health Priority.
Am Med Dir Assoc. 2016 Jan 21. pii: S1525-8610(15)00766-5.
doi: 10.1016/j.jamda.2015.12.016. [Epub ahead of print]
4. Ain S, Maz?c?oglu MM, Mucuk S, Gocer S, Deniz ?afak
E, Arguvanl? S, Ozturk A. The prevalence of frailty and
related factors in community-dwelling Turkish elderly
according to modified Fried Frailty Index and FRAIL scales.
Aging Clin Exp Res. 2015 Oct;27(5):703-9. doi: 10.1007/s40520-015-0337-0.
Epub 2015 Mar 12.
5. Eyigor S, Kutsal YG, Duran E, Huner B, Paker N, Durmus
B, Sahin N, Civelek GM, Gokkaya K, Do?an A, Günayd?n
R, Toraman F, Cakir T, Evcik D, Aydeniz A, Yildirim AG,
Borman P, Okumus M, Ceceli E; Turkish Society of Physical
Medicine and Rehabilitation, Geriatric Rehabilitation
Working Group. Frailty prevalence and related factors
in the older adult-FrailTURK Project. Age (Dordr). 2015
Jun;37(3):9791. doi: 10.1007/s11357-015-9791-z. Epub 2015
May 7.
6. Çakmur H. Frailty among elderly adults in a
rural area of Turkey. Med Sci Monit. 2015 Apr 30;21:1232-42.
doi: 10.12659/MSM.893400.
7. De Lepeleire J, Iliffe S, Mann E, Degryse JM. Frailty:
An emerging concept for
general practice. Br J Gen Pract 2009;59:e177-182.
8.Prince MJ, Wu F, Guo Y, et al. The burden of disease
in older people and implications for health policy and
practice. Lancet 2015;385:549-562.
9. Walters, K., Iliffe, S., Tai, S. S., & Orrell,
M. (2000). Assessing needs from patient, carer and professional
perspectives: The Camberwell Assessment of Need for Elderly
people in primary care. Age and Ageing, 29, 505-510.
10. Hoogendijk EO, Muntinga ME, van Leeuwen KM, van der
Horst HE, Deeg DJ, Frijters DH, Hermsen LA, Jansen AP,
Nijpels G, van Hout HP. Self-perceived met and unmet care
needs of frail older adults in primary care. Arch Gerontol
Geriatr. 2014 Jan-Feb;58(1):37-42. doi: 10.1016/j.archger.2013.09.001.
Epub 2013 Sep 12.
11. "frailty at a glance. Accessed: 01.01.2016. Accessed
at: http://www.frailty.net/frailty-at-a-glance.
12. Fit for Frailty - consensus best practice guidance
for the care of older people living in community and outpatient
settings - a report from the British Geriatrics Society
2014.
13. Yaman A, Yaman H. Frailty in Family Practice: Diagnosis
and Management (in Turkish). Ankara Med J, 2015, 15(2):89-95.
14. Morley JE, Cao L. Rapid screening for sarcopenia.
J Cachexia Sarcopenia Muscle. 2015 Dec; 6(4): 312-314.
Published online 2015 Nov 18. doi: 10.1002/jcsm.12079
15. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm
T, Landi F, et al. Sarcopenia: European consensus on definition
and diagnosis: report of the European Working Group on
Sarcopenia in Older People. Age Ageing 2010; 39: 412-423.
16. Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley
JE, Newman AB, et al. Sarcopenia: an undiagnosed condition
in older adults. Current consensus definition: prevalence,
etiology, and consequences. International Working Group
on Sarcopenia. J Am Med Dir Assoc 2011; 12: 249-256.
17. Malmstrom TK, Miller DK, Simonsick EM, Ferrucci L,
Morley JE. SARC-F: a symptom score to predict persons
with sarcopenia at risk for poor functional outcomes.
Journal of Cachexia, Sarcopenia and Muscle 2015; DOI:
10.1002/jcsm.12048
18. Heckman G, Molnar FJ.Frailty: Identifying elderly
patients at high risk of poor outcomes. Can Fam Physician.
2015 Mar;61(3):227-31.
19. Lee L, Heckman G, Molnar FJ. Frailty: Identifying
elderly patients at high risk of poor outcomes. Can Fam
Physician. 2015 Mar;61(3):227-31.
20. McKenzie K, Ouellette-Kuntz H, Martin L. Using an
accumulation of deficits approach to measure frailty in
a population of home care users with intellectual and
developmental disabilities: an analytical descriptive
study. BMC Geriatr. 2015 Dec 18;15:170. doi: 10.1186/s12877-015-0170-5.
21. Hoogendijk EO1, Muntinga ME, van Leeuwen KM, van der
Horst HE, Deeg DJ, Frijters DH, Hermsen LA, Jansen AP,
Nijpels G, van Hout HP. Self-perceived met and unmet care
needs of frail older adults in primary care. Arch Gerontol
Geriatr. 2014 Jan-Feb;58(1):37-42. doi: 10.1016/j.archger.2013.09.001.
Epub 2013 Sep 12.
22. Yaman A, Yaman H. The Cognitive Evaluation of Elderly
Individuals in Family Practice. KONURALP TIP DERGISI 2015;
7 (2): 121-123.
23. Ilinca S, Calciolari S. The patterns of health care
utilization by elderly Europeans: frailty and its implications
for health systems. Health Serv Res. 2015 Feb;50(1):305-20.
doi: 10.1111/1475-6773.12211. Epub 2014 Aug 19.
|